Self-Insured Employers
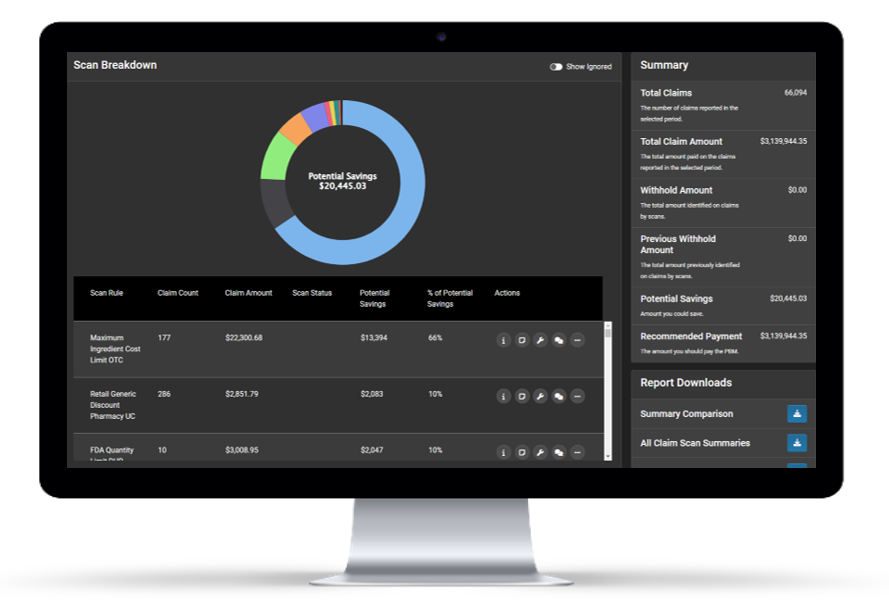
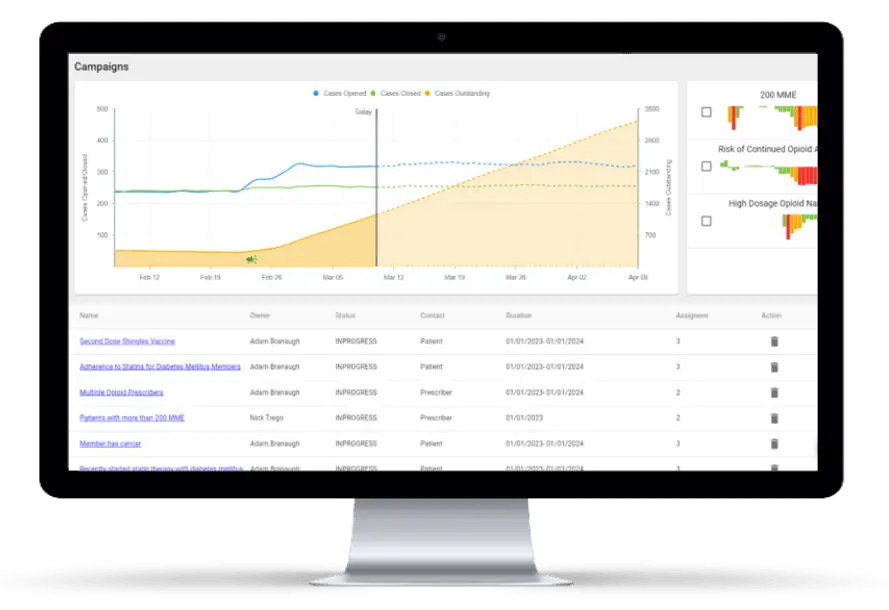
Delivering a robust pharmacy benefit while upholding fiduciary responsibilities is key part of what employers must deliver. With the complexity of pharmacy claims and limited pharmacy resources, benefit oversight can be challenging. HDS makes it easy. With HDS Spotlight, employers can monitor 100% of their claims in real-time to ensure adjudication accuracy according to the benefit design and monitor PBM vendor performance.
Automate the Oversight of Your Prescription Drug Benefit
Identify
HDS proprietary pharmacy analytics technology identifies claim-level errors using 500+ scans in six key domains, including contract errors, plan design, and more.
Fix
Once claim errors are identified, the system prioritizes findings to quickly perform a root cause analysis and expedite a fix.
Monitor
Once a fix has been implemented by the PBM, the HDS Spotlight platform serves to validate the fix was implemented on time and remains in place.
Interested in Adding Continuous Claims Monitoring?
Add the Power Of Advanced Pharmacy Analytics to Your Benefit
Optimize Visibility Into Your Data
Accessing all your pharmacy data can be a challenge. Analyzing it to make strategic decisions can be overwhelming. HDS provides unbiased, third-party pharmacy data analytics that enable employers to see “behind the curtain” into their pharmacy benefit to truly optimize performance.
Validate ERISA Compliance
As a self-funded employer and fiduciary, it is essential to comprehensively monitor prescription spend. HDS Employers are equipped with ongoing claims monitoring to identify errors in adjudication, as well as savings opportunities to ensure your pharmacy benefit stays market competitive.