Solutions
Pharmacy payment integrity
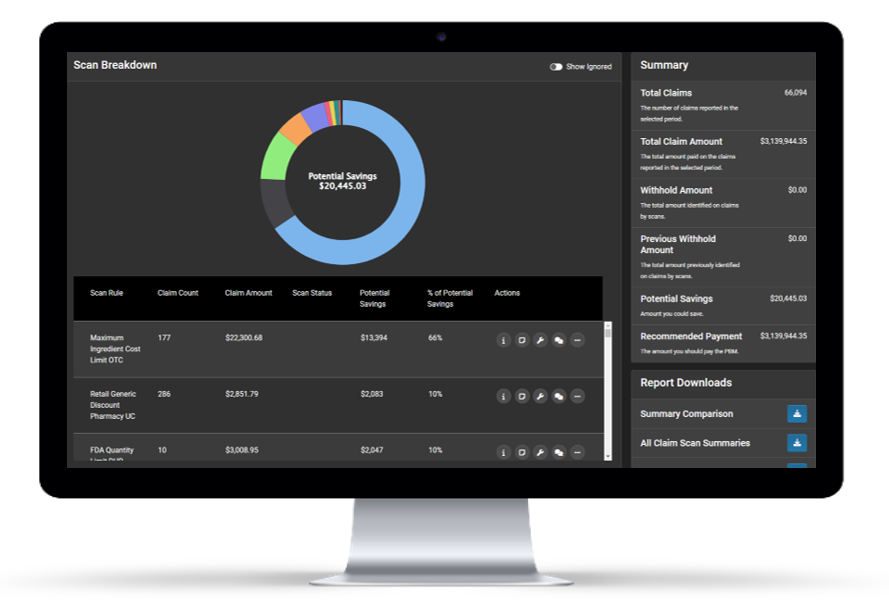
Claim Scan
Claim Scan empowers clients to monitor 100% of their pharmacy claims to identify adjudication errors as they occur, offering the data to support mid-contract amendments, RFP leverage, and realized savings.
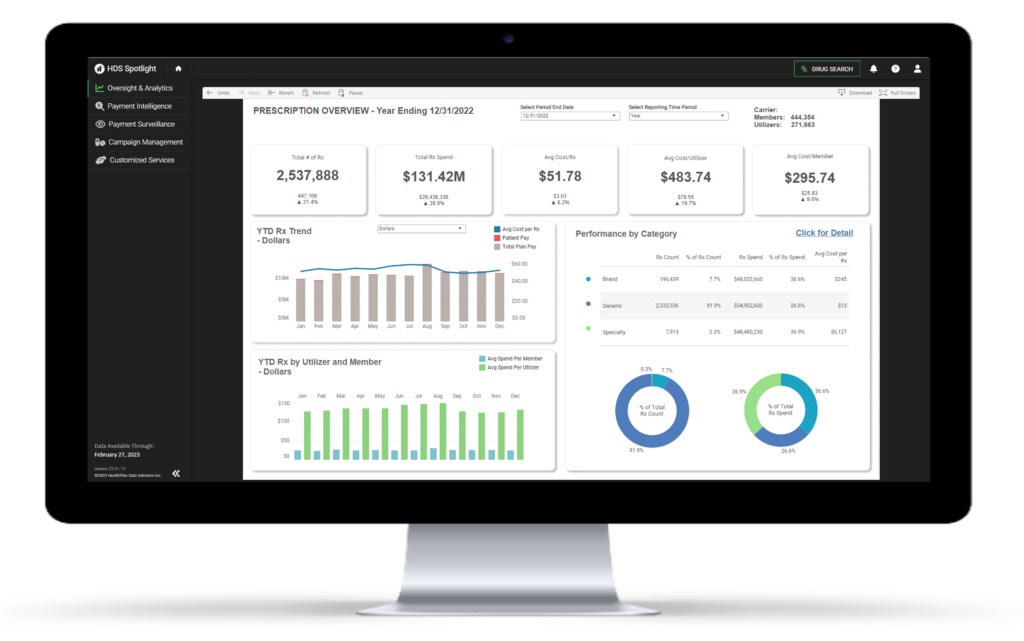
Pharmacy data insights
Rx Oversight and Analytics
Rx Oversight and Analytics provides visibility and insight into pharmacy claim data through customized reporting, querying, dashboarding, and trending capabilities.
Customized services
Pharmacy benefit consulting
Pairing our technology with deep pharmacy benefit expertise enables our team to provide additive value to traditional pharmacy benefit services.
Smarter pharmacy oversight with real-time results

Curb your pharmacy
spend
We help you see exactly where your pharmacy dollars are going. With real-time analytics and actionable insight, we give you the tools to slow rising costs and make smarter use of resources.
Identify and realize
cost savings
Instead of waiting for a retrospective audit, we monitor claims as they happen. Our solutions flag savings opportunities in real time so you can act quickly, recover dollars, and avoid unnecessary spend.

Manage your benefit oversight
in one platform
We bring all of your pharmacy benefit data into one secure, web-based platform. With continuous monitoring and clear reporting, you get the visibility and control to manage benefits effectively.