100% continuous oversight. Smarter pharmacy spend.
We combine clinical logic, contract analytics, and market benchmarks to deliver real-time, actionable insight into your entire pharmacy benefit.
Pharmacy data analytics solutions fortoday's problems

Rising pharmacy costs
Pharmacy costs continue to rise — and so does the pressure to make every dollar count. Ensuring accurate, appropriate claim payments is no longer optional. It’s essential to avoid overspending and deliver measurable value to members.

Ineffective cost savings measures
As pharmacy costs climb, many still depend on audits, market checks, and RFPs to manage spend. But those are post-mortems — not prevention.
Disparate claims monitoring systems
Pharmacy benefit management is complex — and fragmented systems make it harder. Claims data is often siloed, difficult to access, and dependent on IT support. With limited resources, many teams struggle to get the visibility they need to make timely, informed decisions.
Oversight that works, no matter your PBM
Opaque pricing and complex contracts make it hard to know if your pharmacy benefit is working the way it should. As regulators push for more transparency, we help you take control.
We use advanced analytics and AI-driven logic to monitor 100% of your claims, continuously. That means real-time oversight across plan design, contract terms, clinical standards, market benchmarks, and compliance.
No matter which PBM you work with, we help ensure your benefit is delivered as intended — with clarity, accountability, and the insight to act when it matters most.

Go beyond the traditional PBM audit
Annual PBM audits are often designed to confirm compliance — not prevent overspending. While audits may uncover issues, recoveries are rarely guaranteed. In many cases, findings arrive too late to make a financial impact and are simply addressed in the next RFP cycle.
We take a different approach. Instead of looking backward, we help you monitor claims in real time. With invoice-level visibility and continuous oversight, you can spot issues early, make mid-contract adjustments, and reduce waste before it becomes loss.
Our solutions give you the insight to act — and the confidence that your pharmacy dollars are being used where they matter most.
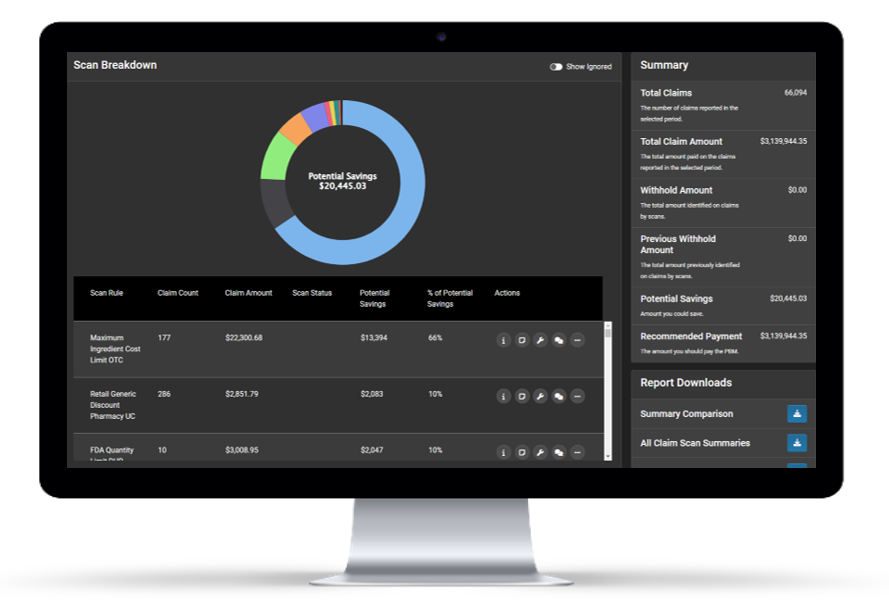
Pharmacy analytics, unified in one platform
Managing pharmacy data often means juggling multiple systems, delayed access, and limited visibility. That fragmentation makes it harder to analyze claims, uncover issues, and act quickly.
We bring everything together in one place — with real-time access, flexible filtering, and intuitive dashboards that make it easy to get the answers you need, when you need them.